This blog is about two of my favorite medical terms: Varus and Valgus. These words come from Latin and they basically are ways to refer to something that is crooked. Most of the time when I use “varus” or “valgus” I am referring to different types of crooked legs. Almost nobody has perfect legs – so most of us fit into the category of either varus or valgus leg alignment.
One of the first things I do when evaluating a new patient is to decide if their legs are varus or valgus. I use these categories as very loose guidelines to help me quickly decide what types of injuries the person might be experiencing. It is not too surprising that people with similar body types often develop similar injuries. Of course there are exceptions to every rule, and there also degrees of severity. Not everyone fits neatly into a category, but I find that this is as good a starting place as any. Here is a brief overview of the Varus, Valgus and “Good” alignment groups.
Before we get too far into this, I need to stop for a disclaimer: Please excuse the poorly hand drawn pictures that resemble happily dancing robots. I am no Picasso. Or maybe I am too much of a Picasso (if you have seen some his cubist paintings).
Good alignment
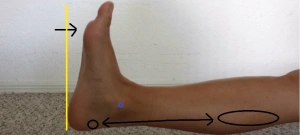
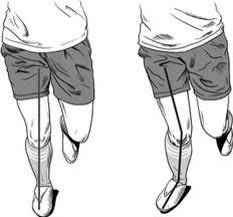
Legs are considered to be in good alignment if a straight line can be drawn from the hip, through the knee to the second toe. Here is a guy with good alignment:
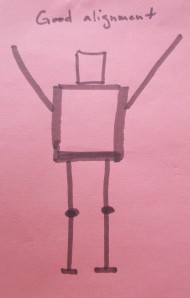
Although this figure looks very smug about his perfect legs, you can’t always assume that people with good leg alignment will be injury free. Legs that are very straight sometimes have a hard time absorbing shock. Because all the bones are aligned exactly on top of each other, every step can send shock waves up into the rest of the body. This shock is often absorbed in the pelvis or spine, resulting in injuries of the back or even the neck.
Varus
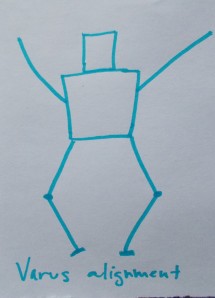
A person with Varus alignment of their legs looks something like this:
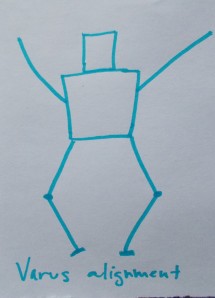
Varus alignment can also be called “Bow legged”. A person with varus alignment has legs that curve outward, with the knee being further out than the foot. The curving shape can happen at either the knee joint itself or because the actual bones of the lower leg are bent outward.
If you have trouble remembering the meaning of varus, remember that that R stands for Rounded.
Varus legs are susceptible to the following injuries:
– Osteoarthritis of the knee
– Shin splints
– IT band pain at the hip or knee
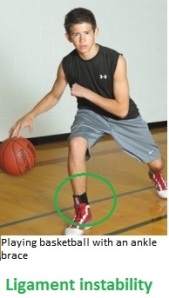
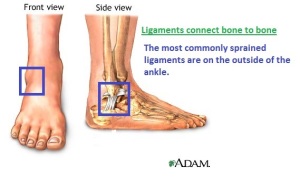
– Chronic ankle sprains
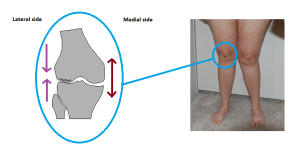
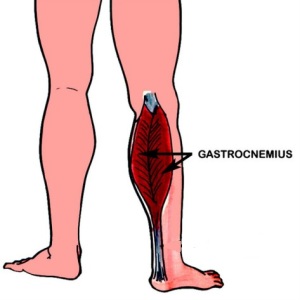
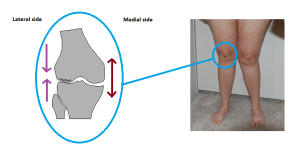
The most common issue I see with people who have varus legs is knee pain. The varus leg shape is bad for both the medial (part on the big toe side) and lateral (part on the pinky toe side) areas of the knee. Because of the curved shape of the leg, all of the structures on the medial side of the knee are squished together and all of the things on the lateral side get stretched apart.
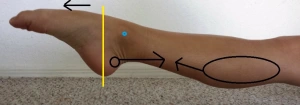
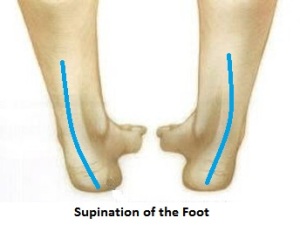
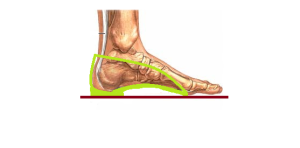
To make matters worse for the varus leg group, it is very common for someone with a varus knee to also have a varus foot alignment. This is also called having a supinated foot. Supinated feet look like this:
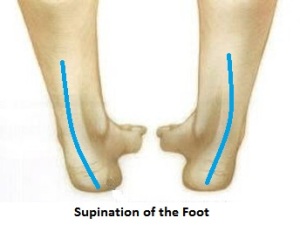
There is a whole list of additional problems that comes with having supinated feet. It will be the subject of its own blog post in the future. For now it is enough to say that people with supinated feet are more likely to sprain their ankles, since they put most of their body weight on the outsides of their feet.
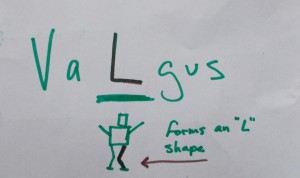
Valgus
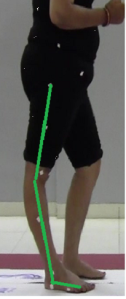
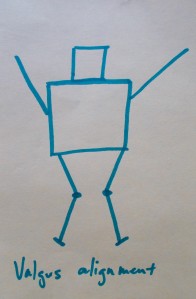
Valgus leg alignment is much more common that varus leg alignment. Someone with valgus legs stands with their knees close together, in a “knock knee” position.
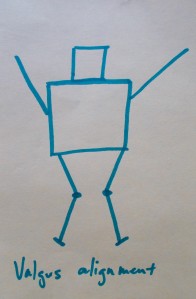
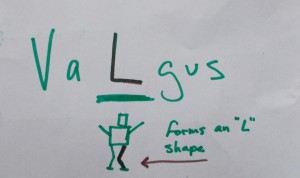
You can remember the term valgus because the leg forms an angle like the letter L
Valgus leg shapes can lead to the following injuries:
– Knee caps that dislocate
– Medial knee pain
– Patella/femoral syndrome (also called jumper’s knee)
– Foot and arch pain
– Low back pain
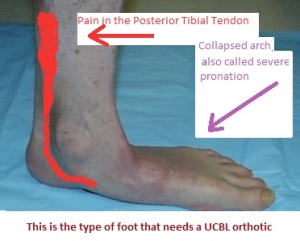
People with valgus leg alignment almost always have pronated feet.
This means that the weight of the body causes the arch of the foot to collapse and the person then stands with more weight on the inside portion of the foot.

Valgus knee alignment (not surprisingly) puts exactly the opposite stresses on the knee as varus alignment does. The lateral side of the knee is squished and the medial side of the knee is stretched.
People with valgus leg alignment often have pain in the front and the inside of their knees. This is because the angle of the leg causes an uneven pull on the kneecap. It is slightly more common for females to have a valgus leg shape because they tend to have wider hips.
The Combo:
It is also possible to have any combination of leg alignments:
One leg could be valgus while the other leg is straight, one leg could be varus with the other leg is straight, or you could even have one of each! These combo arrangements often happen either as the result of a serious injury (like a fracture that didn’t heal well) or because one leg is significantly longer than the other.
So what should you do if you have varus or valgus legs?
– Loose the extra weight. If you have varus or valgus leg alignment, the best thing you can do for yourself is to maintain a healthy body weight. Additional pounds can make a mild alignment issue much worse. Our legs have to work really hard to support us, even under the best of circumstances. People who naturally have excellent body alignment can often get away with being a bit heavier, but anyone who has varus or valgus legs should be very cautions not to make the issue more severe by gaining too much weight.
– Do low impact exercises and activities. The stress associated with long distance running and other such repetitive activities can really prove damaging to people who have severe varus or valgus alignments. Cross training and alternative exercise programs are a great way to overcome this. Try swimming or biking for your cardio workouts. You can still do some running, just keep it in moderation.
– You might be able to somewhat improve your alignment by doing specially targeted stretching and strengthening exercises. Find yourself a physical therapist or fitness specialist who can help you set up a routine.
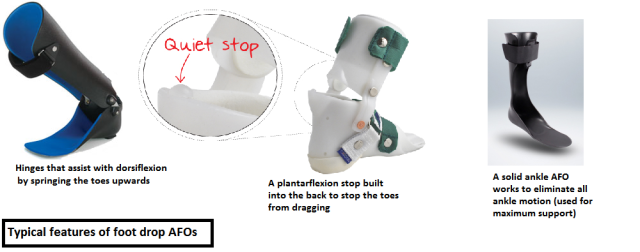
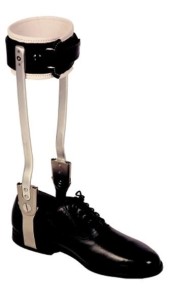
– Sometimes the alignment issue is severe enough that a brace must be used on that leg. “Unloading” knee braces apply force to the side of the knee in an effort to reduce the angle of the joint.
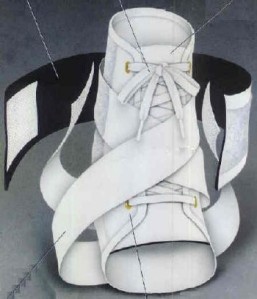
– Foot orthotics can correct the issue from the ground up – this can often reduce the amount of varus or valgus in the rest of the leg.
– Remember that poor body alignment can lead to chronic injuries. Be careful with yourself! If you do develop one of these injuries, be sure that you treat it and allow it to fully heal so that it won’t come back to haunt you. Sometimes this means changing your usual activities… I’m looking at you, distance runners!
– If the alignment problem is severe enough you will probably be referred to see an orthopedic surgeon. The orthopedic surgeon might tell you that a knee replacement surgery is in your future.
** Remember that surgeons make their living by doing surgeries – it is always ok to get a second opinion from someone who doesn’t stand to benefit from performing an operation on you. **
Walk well!


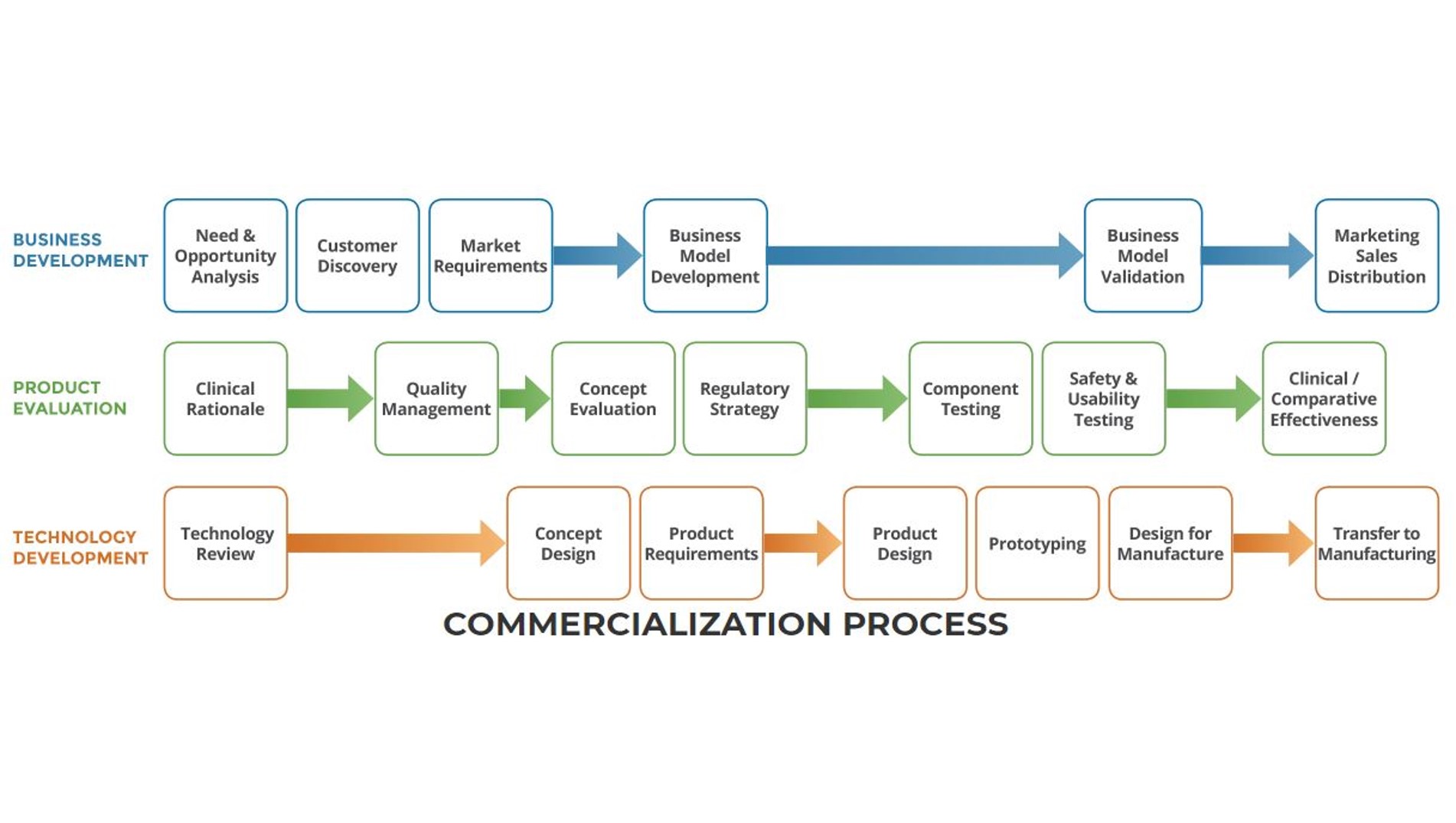
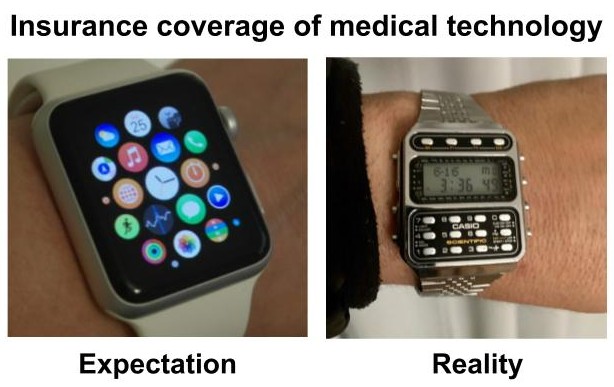 There are huge advantages to the new “smart device” revolution that is sweeping the medical technology world. Including but not limited to:
There are huge advantages to the new “smart device” revolution that is sweeping the medical technology world. Including but not limited to: 
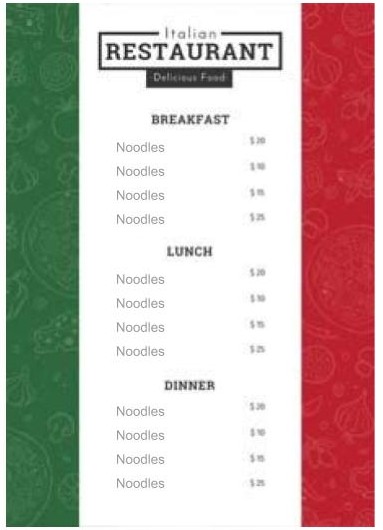 That is like my very non-Italian grandfather on my father’s side driving my very Italian mother up the wall by referring to all pasta (no matter the size, shape, or ingredients) as “noodles”. It could be any dish from fettuccine alfredo to lasagna and it would all just be “noodles” to him. This limited vocabulary obscures communication and it is very frustrating! Imagine a restaurant menu that used this system. Chaos would ensue.
That is like my very non-Italian grandfather on my father’s side driving my very Italian mother up the wall by referring to all pasta (no matter the size, shape, or ingredients) as “noodles”. It could be any dish from fettuccine alfredo to lasagna and it would all just be “noodles” to him. This limited vocabulary obscures communication and it is very frustrating! Imagine a restaurant menu that used this system. Chaos would ensue.